Demystifying the New CMS Prior Authorization Rule
The healthcare landscape is evolving rapidly, driven by a focus on streamlining processes, empowering patients, and delivering quality care efficiently. The new prior authorization rule, with its emphasis on the HL7 FHIR data integration standard, is a pivotal step in this direction. But navigating these complexities can be challenging for healthcare providers and payers alike.
This is where Falkondata, with its expertise in healthcare data integration and interoperability, comes in as your trusted partner.
Here are some frequently asked questions about this new rule:
Q: What is the new rule by the Centers for Medicare & Medicaid Services (CMS) about?
A: The new rule by CMS is about improving healthcare data exchange and prior authorization processes. It aims to streamline the prior authorization process, improve data exchange between providers and payers, and give patients more access to their health information. The new rule requires payers to support HL7 FHIR® Prior Authorization API data integration standard and/or X12 278 transaction standard.
Q: How will the HL7 FHIR Prior Authorization API improve the process?
A: This API automates the entire prior authorization process electronically, saving time and reducing administrative burden for both providers and payers. Medicare FFS already uses this API successfully, demonstrating its efficiency.
Q: What about the X12 278 standard? Is it mandatory?
A: While the rule encourages the use of FHIR API, it offers flexibility. Payers who implement a fully FHIR-based API won’t be penalized for not using X12 278, allowing them to choose an FHIR-only or combined approach. They can also offer an X12-only option if desired.
Q: What other API requirements are included?
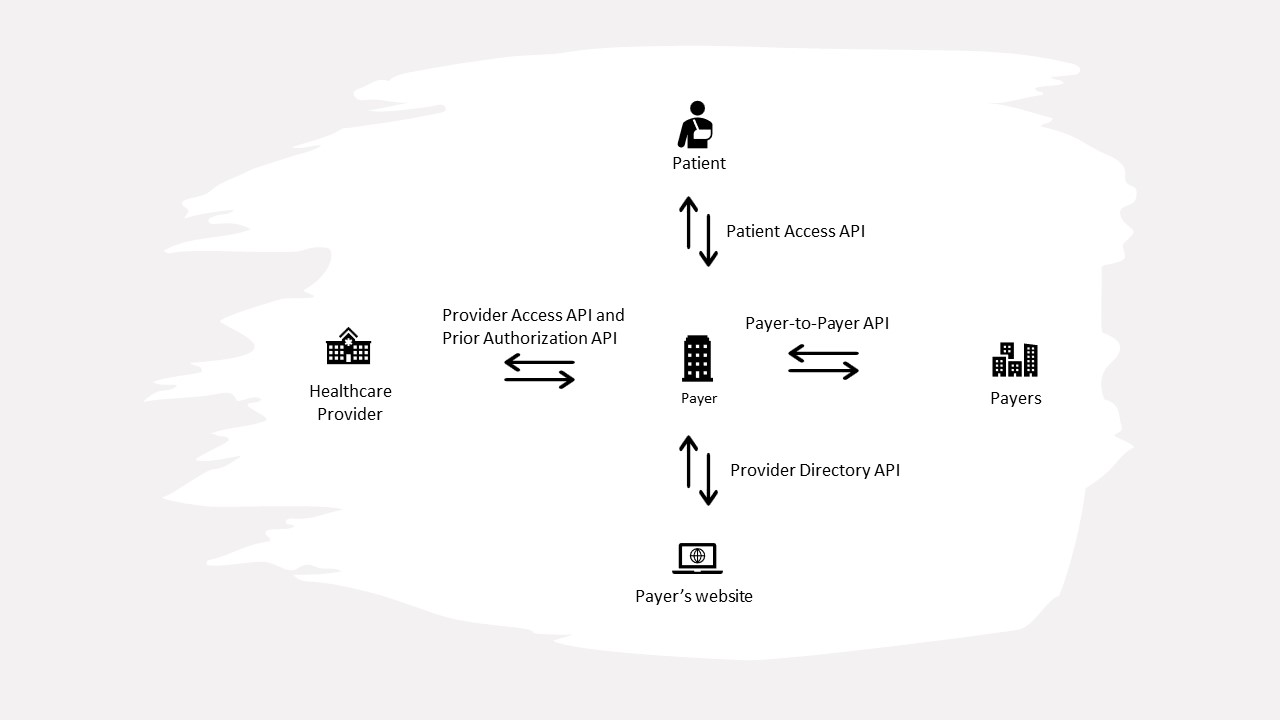
A: By January 2027, payers must:
- Expand their Patient Access API to include prior authorization information.
- Implement a Provider Access API for data retrieval (claims, encounters, clinical data, prior authorizations).
- Exchange patient data (with permission) via Payer-to-Payer FHIR API when patients switch payers or have multiple ones.
Here are all the APIs healthcare payers should implement:
Here is a link to the chart of proposed and current API standards.
Q: How will these changes benefit patients and providers?
A: These data integration efforts aim to:
- Reduce administrative burden for healthcare professionals.
- Allow clinicians to spend more time on direct patient care.
- Prevent delays in care for patients needing prior authorization.
- Improve access to health information for patients and providers.
Q: What about the enforcement of these standards?
A: HHS will enforce the use of the FHIR API for prior authorization. However, they offer enforcement discretion for the X12 278 standard, allowing flexibility in implementation.
Q: Is there anything else to know about this rule?
A: The API compliance deadline has been delayed from January 2026 to January 2027 due to public feedback. Additionally, a new Electronic Prior Authorization measure is being added to MIPS and the Medicare Promoting Interoperability Program to track API usage.
By implementing these standards and promoting data exchange, the goal is to create a more efficient prior authorization process, improve access to health information, and ultimately deliver better, timelier care to patients.
Q. How can Falkondata help with this new rule?
A: The new healthcare rule mandates data integration standards like HL7 FHIR and X12 278 to revolutionize prior authorization, but navigating these complexities can be daunting. That’s where Falkondata steps in.
We are healthcare data integration experts:
- Proven track record: Successfully implemented various FHIR, HL7 messages, and X12 interfaces.
- Deep understanding: We grasp provider and payer workflows for seamless integration.
- Comprehensive service: We help implement provider, patient, and prior authorization APIs, ensuring compliance and efficiency.
Embrace the benefits:
- Reduce administrative burden: Free up valuable time for healthcare professionals.
- Empower patients: Enhance access to health information and faster care delivery.
- Boost efficiency: Streamline prior authorization processes with automated solutions.
Don’t wait to adapt. Contact Falkondata today to discuss your project and:
- Simplify compliance: Ensure smooth implementation of data integration standards.
- Optimize workflows: Enhance provider and payer communication for better patient care.
- Unlock the future: Embrace the evolving healthcare landscape with confidence.
Together, let’s build a more efficient and patient-centric healthcare system.

